The greater impact, however, seems to be the effect the surgery has on gut hormones that impact a number of factors including hunger, satiety, and blood sugar control. Short term studies show that the sleeve is as effective as the roux-en-Y gastric bypass in terms of weight loss and improvement or remission of diabetes. There is also evidence that suggest the sleeve, similar to the gastric bypass, is effective in improving type 2 diabetes independent of the weight loss.
- protein lose body fat.
- fasting jumpstart weight loss.
- do i need to lose weight to run faster.
- More on this topic for:!
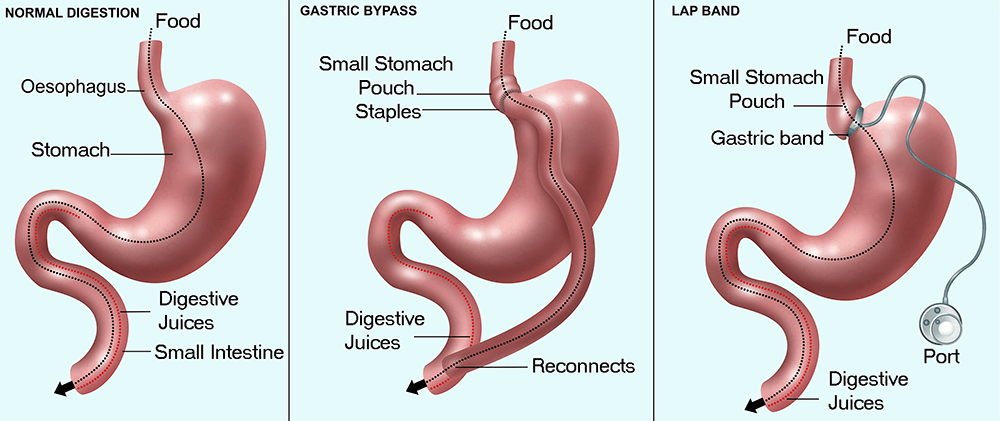
The complication rates of the sleeve fall between those of the adjustable gastric band and the roux-en-y gastric bypass. The Adjustable Gastric Band — often called the band — involves an inflatable band that is placed around the upper portion of the stomach, creating a small stomach pouch above the band, and the rest of the stomach below the band. The common explanation of how this device works is that with the smaller stomach pouch, eating just a small amount of food will satisfy hunger and promote the feeling of fullness.
Share via email
The feeling of fullness depends upon the size of the opening between the pouch and the remainder of the stomach created by the gastric band. The size of the stomach opening can be adjusted by filling the band with sterile saline, which is injected through a port placed under the skin. What is known is that there is no malabsorption; the food is digested and absorbed as it would be normally. The clinical impact of the band seems to be that it reduces hunger, which helps the patients to decrease the amount of calories that are consumed.
First, a smaller, tubular stomach pouch is created by removing a portion of the stomach, very similar to the sleeve gastrectomy. Next, a large portion of the small intestine is bypassed. The duodenum, or the first portion of the small intestine, is divided just past the outlet of the stomach.
Bariatric surgery
A segment of the distal last portion small intestine is then brought up and connected to the outlet of the newly created stomach, so that when the patient eats, the food goes through a newly created tubular stomach pouch and empties directly into the last segment of the small intestine. Roughly three-fourths of the small intestine is bypassed by the food stream. The bypassed small intestine, which carries the bile and pancreatic enzymes that are necessary for the breakdown and absorption of protein and fat, is reconnected to the last portion of the small intestine so that they can eventually mix with the food stream.
Unlike the other procedures, there is a significant amount of small bowel that is bypassed by the food stream.
- ketogenic diet example plan.
- Weight Loss Surgery.
- Types of Bariatric Surgery.
- gnc weight loss programs that fit.
Additionally, the food does not mix with the bile and pancreatic enzymes until very far down the small intestine. This results in a significant decrease in the absorption of calories and nutrients particularly protein and fat as well as nutrients and vitamins dependent on fat for absorption fat soluble vitamins and nutrients. Update your browser to view this website correctly.
Open surgery may be a better option for certain people. If you have a high level of obesity , have had stomach surgery before, or have other complex medical problems, you may need open surgery. In this type of surgery, the surgeon places a ring with an inner inflatable band around the top of your stomach to create a small pouch. This makes you feel full after eating a small amount of food. The band has a circular balloon inside that is filled with salt solution.
The surgeon can adjust the size of the opening from the pouch to the rest of your stomach by injecting or removing the solution through a small device called a port placed under your skin.
Weight Loss Surgery (for Parents) - Nemours KidsHealth
After surgery, you will need several follow-up visits to adjust the size of the band opening. If the band causes problems or is not helping you lose enough weight, the surgeon may remove it. The U. Food and Drug Administration FDA has approved use of the gastric band for people with a BMI of 30 or more who also have at least one health problem linked to obesity, such as heart disease or diabetes. In gastric sleeve surgery, also called vertical sleeve gastrectomy, a surgeon removes most of your stomach, leaving only a banana-shaped section that is closed with staples.
Like gastric band surgery, this surgery reduces the amount of food that can fit in your stomach, making you feel full sooner. Taking out part of your stomach may also affect gut hormones or other factors such as gut bacteria that may affect appetite and metabolism. This type of surgery cannot be reversed because some of the stomach is permanently removed.
Gastric bypass surgery, also called Roux-en-Y gastric bypass, has two parts. First, the surgeon staples your stomach, creating a small pouch in the upper section.
Guide to bariatric surgery
The staples make your stomach much smaller, so you eat less and feel full sooner. Next, the surgeon cuts your small intestine and attaches the lower part of it directly to the small stomach pouch.
Food then bypasses most of the stomach and the upper part of your small intestine so your body absorbs fewer calories. The surgeon connects the bypassed section farther down to the lower part of the small intestine. This bypassed section is still attached to the main part of your stomach, so digestive juices can move from your stomach and the first part of your small intestine into the lower part of your small intestine.
The bypass also changes gut hormones, gut bacteria, and other factors that may affect appetite and metabolism. Gastric bypass is difficult to reverse, although a surgeon may do it if medically necessary. This surgery, also called biliopancreatic diversion with duodenal switch, is more complex than the others.
The duodenal switch involves two separate surgeries. The first is similar to gastric sleeve surgery. The second surgery redirects food to bypass most of your small intestine. The surgeon also reattaches the bypassed section to the last part of the small intestine, allowing digestive juices to mix with food.
This type of surgery allows you to lose more weight than the other three. However, this surgery is also the most likely to cause surgery-related problems and a shortage of vitamins, minerals, and protein in your body. For these reasons, surgeons do not perform this surgery as often.
NHS weight loss surgery
Surgeon places an inflatable band around top part of stomach, creating a small pouch with an adjustable opening. Surgeon staples top part of stomach, creating a small pouch and attaching it to middle part of small intestine. Adapted from: Bariatric surgery procedures. Accessed May 24, Image credit: Walter Pories, M. Before surgery, you will meet with several health care providers, such as a dietitian , a psychiatrist or psychologist, an internist, and a bariatric surgeon.
These health care providers also will advise you to become more active and adopt a healthy eating plan before and after surgery. In some cases, losing weight and bringing your blood sugar levels closer to normal before surgery may lower your chances of having surgery-related problems. Some bariatric surgery programs have groups you can attend before and after surgery that can help answer questions about the surgery and offer support.
After surgery, you will need to rest and recover. Although the type of follow-up varies by type of surgery, you will need to take supplements that your doctor prescribes to make sure you are getting enough vitamins and minerals. Walking and moving around the house may help you recover more quickly. As you feel more comfortable, add more physical activity. After surgery, most people move from a liquid diet to a soft diet such as cottage cheese, yogurt, or soup, and then to solid foods over several weeks.
Your doctor, nurse, or dietitian will tell you which foods and beverages you may have and which ones you should avoid. You will need to eat small meals and chew your food well.